Neovascular age-related macular degeneration (nAMD) is one of the leading causes of vision loss, and managing it often means frequent eye injections. In real-world settings, patients average around five intravitreal anti-VEGF injections in the first year, with slightly fewer in the second. While these treatments are effective, the requirement for repeated visits creates a substantial burden for patients, their families, and healthcare systems.
To ease this challenge, researchers have developed newer therapies designed to last longer between doses. One of the most significant recent advances is Vabysmo (faricimab-svoa) — the first treatment of its kind to block two pathways simultaneously. By targeting both VEGF-A and Ang-2, Vabysmo helps control abnormal blood vessel growth and leakage in the retina, which are the root problems behind diseases like nAMD.
In this article, we’ll learn what Vabysmo is, explain how it works, outline its benefits, and compare it with other available anti-VEGF options. Whether you’re a patient, caregiver, or healthcare professional, this guide will provide a clear picture of where Vabysmo fits into modern eye care.
Key Takeaways
- Vabysmo (faricimab-svoa) is the first intravitreal drug to block two disease pathways in the retina: VEGF-A and Ang-2. This dual action improves vascular stability and helps reduce fluid buildup.
- The FDA approved Vabysmo in 2022 for wet AMD and DME, with an expanded approval in 2023 for macular edema following retinal vein occlusion (RVO).
- In large trials (TENAYA, LUCERNE, YOSEMITE, RHINE), Vabysmo proved non-inferior to Eylea for vision outcomes, with many patients able to extend dosing intervals to 12–16 weeks—though not all achieve the longest interval.
- Safety profile is consistent with other intravitreal anti-VEGF injections. The most common side effect is conjunctival hemorrhage (~7%), while rare but serious risks include endophthalmitis and retinal detachment.
- Compared with older therapies, Vabysmo represents a notable advance in reducing treatment burden while maintaining strong visual outcomes.
- For patients, it offers the potential for fewer injections, less clinic time, and improved long-term disease control, making it a significant new option in retinal care.
About: Doctor Medica is your trusted supplier of top-quality dermal fillers, viscosupplements, and more for your medical practice. We offer genuine products from leading brands at the lowest prices in the market. If you’re looking to order Vabysmo online for your practice, contact Doctor Medica today.
Mechanism of Action of Vabysmo in Retinal Therapy

The effectiveness of Vabysmo (faricimab-svoa) comes from its ability to block two critical pathways involved in retinal disease. Like older drugs, it targets VEGF-A, the main driver of abnormal blood vessel growth and fluid leakage in the retina. At the same time, it inhibits Angiopoietin-2 (Ang-2), a protein that destabilizes blood vessels and contributes to vascular leakage.
By acting on both VEGF-A and Ang-2, Vabysmo helps improve vascular stability and reduce retinal swelling, resulting in clearer, more consistent vision. While preclinical evidence suggests that Ang-2 inhibition may also influence inflammation, the FDA label notes that its contribution to clinical outcomes has not yet been fully established. This caveat is crucial when considering how Vabysmo works in comparison to single-pathway therapies.
For patients and clinicians, the benefit of this dual mechanism lies in the potential for longer treatment intervals and stronger anatomical control. Not every patient will achieve maximum extension intervals, but the science behind dual inhibition underscores why Vabysmo is viewed as a notable advance in ophthalmology.
FDA-Approved Indications for Vabysmo

The U.S. Food and Drug Administration (FDA) approved Vabysmo in 2022, marking a milestone in retinal therapy. Since then, its indications have expanded: as of October 2023, Vabysmo is approved for neovascular (wet) age-related macular degeneration (nAMD), diabetic macular edema (DME), and macular edema following retinal vein occlusion (RVO). This broader approval provides patients and ophthalmologists with more options for managing vision-threatening conditions.
Indications
- Wet AMD: A leading cause of severe vision loss in adults over 60. It occurs when abnormal blood vessels grow under the retina and leak fluid, resulting in scarring and damage to central vision. By targeting two disease pathways, Vabysmo helps slow this process and preserve sight.
- Diabetic Macular Edema (DME): A diabetic complication where fluid accumulates in the macula, the part of the retina responsible for sharp central vision. Vabysmo reduces this swelling and helps maintain functional vision.
- Retinal Vein Occlusion (RVO): Caused by blocked retinal veins, which lead to swelling and bleeding. Vabysmo’s approval for macular edema after RVO expands its role beyond AMD and DME, showing promise in a broader spectrum of retinal vascular conditions.
This wider approval means Vabysmo is now part of the ongoing discussion of Vabysmo vs Eylea, offering doctors flexibility to tailor therapy based on disease type, dosing needs, and patient preferences.
Vabysmo Clinical Trial Evidence and Efficacy Data
Vabysmo’s approval was built on evidence from large, multicenter phase 3 trials. The TENAYA and LUCERNE studies in wet AMD showed that Vabysmo was non-inferior to Eylea in maintaining vision, with many patients extending treatment intervals to 12–16 weeks. Similarly, the YOSEMITE and RHINE studies in DME demonstrated comparable visual outcomes with fewer injections over time.
Key findings include:
- Visual Outcomes: Both drugs delivered strong gains in best-corrected visual acuity (BCVA), confirming Vabysmo’s ability to match the standard set by Eylea.
- Durability: A significant proportion of Vabysmo patients were able to maintain extended dosing intervals of 12–16 weeks, although extension success varied by baseline disease activity, and not all patients achieved maximum spacing.
- Fluid Control: In some analyses, Vabysmo demonstrated greater reductions in central retinal thickness compared to Eylea. However, this was not consistent across all studies.
Safety data from clinical trials showed that the most common adverse event was conjunctival hemorrhage (~7%). Other possible post-injection effects include eye discomfort or temporary blurred vision, although these are not among the most frequently reported events in trials. Rare but serious complications such as endophthalmitis and retinal detachment were reported, consistent with the risks of all intravitreal injections.
Together, these results reinforce Vabysmo as a therapy that strikes a balance between efficacy and reduced treatment burden, making it a valuable addition to long-term retinal care.
Dosing and Administration Guidelines for Vabysmo
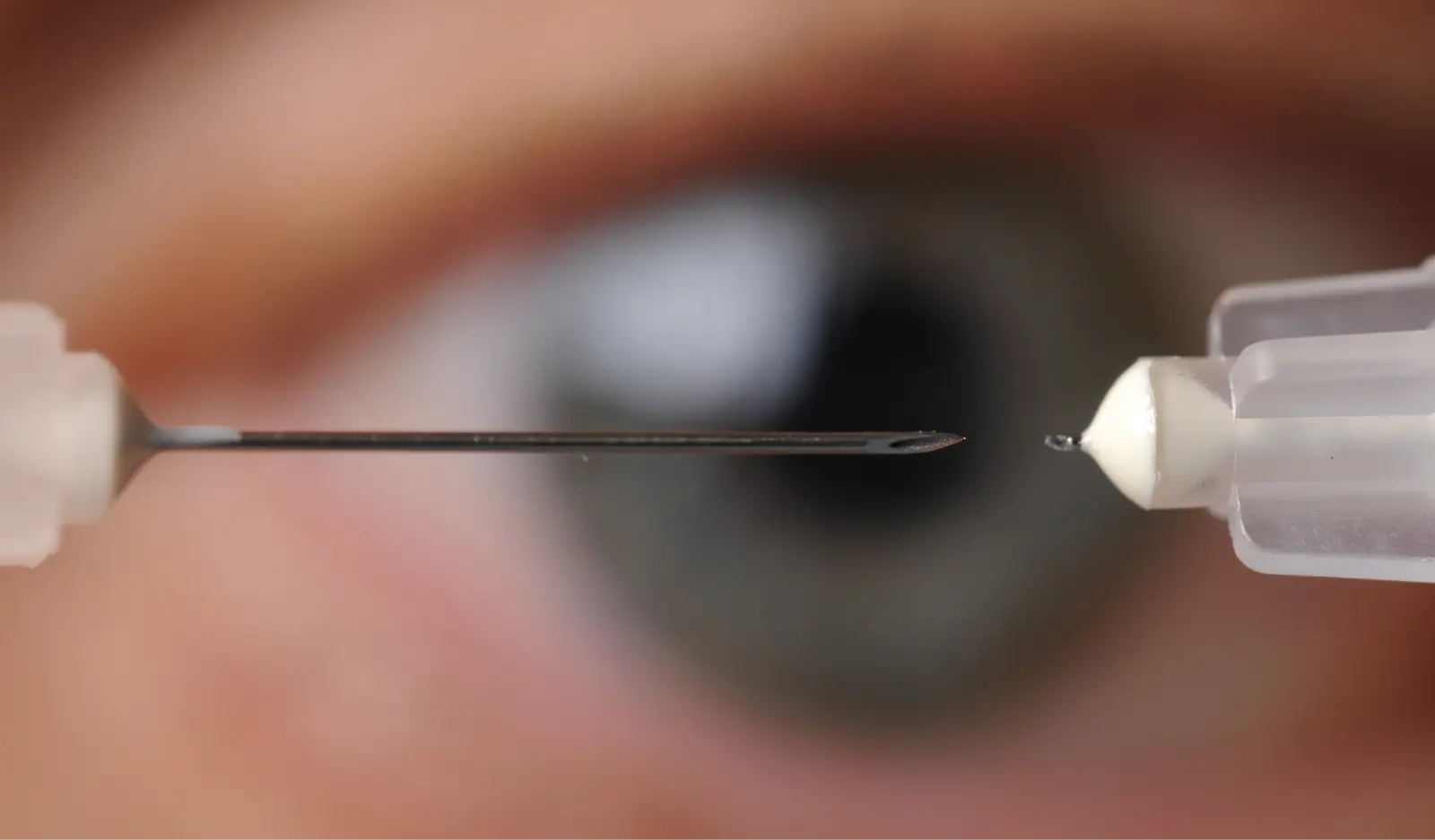
Vabysmo is given as an intravitreal injection by an ophthalmologist under sterile conditions. Treatment begins with an initial loading phase, followed by tailored intervals based on disease activity.
Dosing Details
- Loading Phase: One injection every month for the first four months.
- Maintenance Phase: Intervals extended to 8, 12, or 16 weeks depending on the patient’s response.
- Administration: Always performed in-office under sterile precautions.
This dosing flexibility enables doctors to tailor treatment schedules to meet individual needs. In trials, many patients maintained vision stability with dosing every 12–16 weeks. However, in real-world practice, the extension depends on both anatomical and functional outcomes. For elderly patients or those with diabetes, the potential to reduce clinic visits is a meaningful advantage, helping preserve quality of life while ensuring effective disease control.
Compared with older therapies, Vabysmo’s longer dosing intervals are a significant step forward. Reducing the physical and emotional burden of frequent injections supports better long-term adherence and outcomes.
Conclusion
Vabysmo represents a significant advancement in retinal therapy, combining VEGF-A and Ang-2 inhibition in a single treatment. With FDA approvals for wet AMD, DME, and RVO, it offers strong efficacy, the possibility of extended dosing intervals, and a safety profile consistent with established anti-VEGF therapies.
For patients, understanding what Vabysmo is goes beyond knowing the name of a drug—it means recognizing how it differs from traditional treatments, what benefits it offers, and what to expect in terms of dosing and follow-up care. For ophthalmologists, it expands the toolkit available to balance effectiveness, convenience, and patient preference in chronic eye disease management.
FAQs
1. What is Vabysmo used for?
Vabysmo is FDA-approved for wet AMD, DME, and macular edema following retinal vein occlusion (RVO).
2. How does Vabysmo differ from Eylea?
Both drugs treat similar retinal diseases, but Vabysmo targets two pathways—VEGF-A and Ang-2—while Eylea blocks VEGF-A, VEGF-B, and PlGF. This difference may allow some patients on Vabysmo to go longer between injections.
3. What are the common Vabysmo side effects?
The most common trial-reported event was conjunctival hemorrhage (~7%). Other possible post-injection effects include temporary eye discomfort or blurred vision. Rare but serious risks include infection inside the eye or retinal detachment.
4. How often do patients receive Vabysmo injections?
Patients start with monthly injections for four months, then may shift to every 8, 12, or 16 weeks depending on treatment response. Not all patients reach the longest interval, but reducing injection frequency is an important benefit of Vabysmo therapy.
References
Korobelnik JF, Delcourt C, Creuzot-Garcher C, et al. Real-life management of neovascular age-related macular degeneration (nAMD) in France: a nationwide observational study using retrospective claims data. J Med Econ. 2021;24(1):1087-1097. doi:10.1080/13696998.2021.1971416
Erie JC, Barkmeier AJ, Hodge DO, Mahr MA. High Variation of Intravitreal Injection Rates and Medicare Anti-Vascular Endothelial Growth Factor Payments per Injection in the United States. Ophthalmology. 2016;123(6):1257-1262. doi:10.1016/j.ophtha.2016.02.015
Related Articles
Joanna Carr
Teosyal Cheek Fillers – Define and Enhance
Teosyal dermal fillers are a popular choice for cheek enhancement, providing volume and contour for a more youthful and balanced appearance.
Joanna Carr
Ellanse Tear Trough – Filling and Smoothing
Ellanse is a dermal filler used to treat tear troughs. It provides a non-surgical solution to fill and smooth this delicate area.
Joanna Carr
PRX-T33 Before and After – With a Photo Gallery
See real PRX-T33 before and after results in our curated photo gallery, showcasing skin improvements in texture, tone, and radiance across different s...


